Understanding Postpartum Depression: Signs, Symptoms, and How to Cope
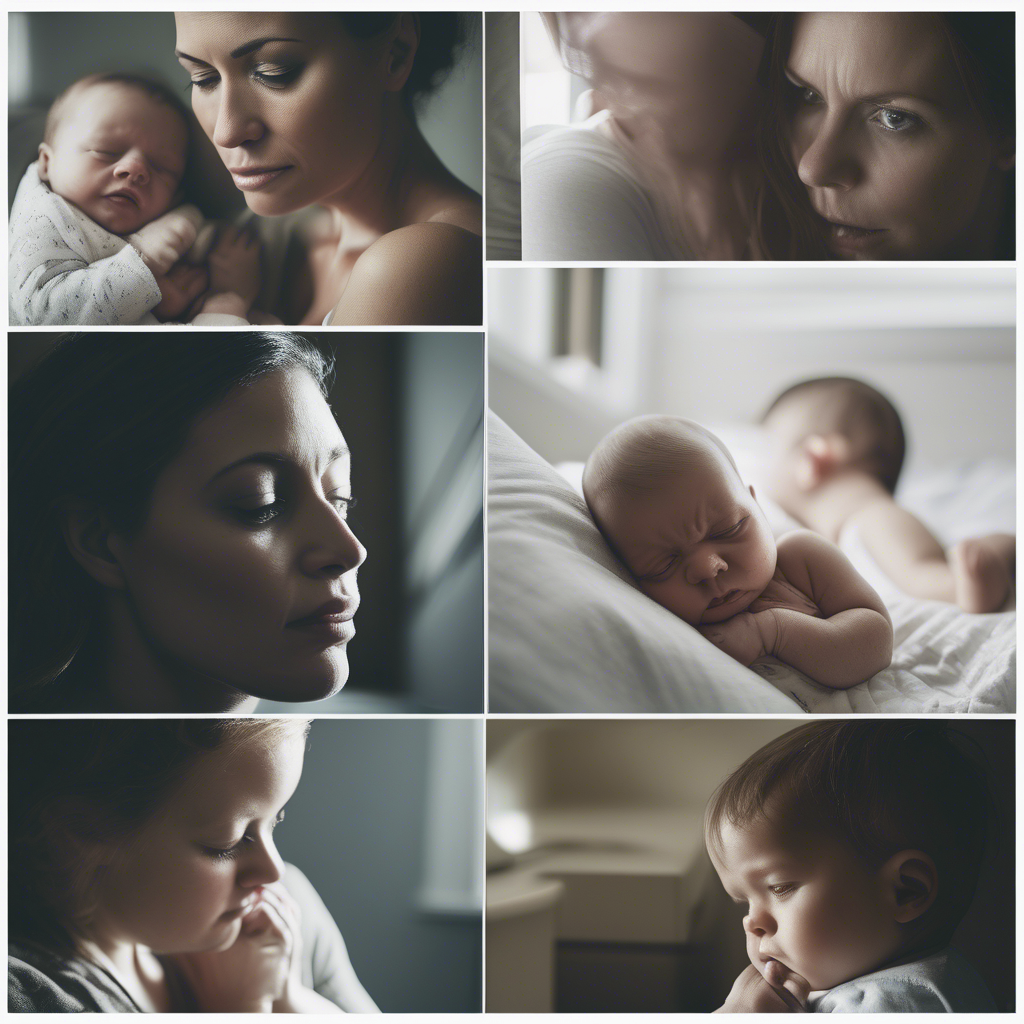
Bringing a new life into the world is often portrayed as a time of joy and excitement. However, for many new mothers, the postpartum period can also be a time of unexpected emotional upheaval. Postpartum depression is a significant mental health issue that affects approximately 1 in 7 women after childbirth. Understanding its signs, symptoms, and how to effectively cope with it is crucial for both mothers and their support networks.
Postpartum depression can deeply impact a mother’s ability to care for her newborn and herself. The societal pressure to embrace motherhood with unbridled happiness often leaves women feeling isolated and ashamed of their struggles. By shedding light on this topic, we aim to normalize these experiences and provide actionable strategies for those affected. This article will explore the various dimensions of postpartum depression, focusing on recognizing the signs, understanding the symptoms, and providing practical coping mechanisms.
In the following sections, you will learn about the critical indicators of postpartum depression, delve into the complexities of its symptoms, and discover effective ways to manage and overcome these challenges. We will also provide insights into best practices for healing after a C-section, a context that often exacerbates postpartum mental health issues.
Recognizing the Signs of Postpartum Depression
Identifying postpartum depression signs can be challenging, as they often overlap with the typical stress and exhaustion of new parenthood. However, distinguishing between the “baby blues” and more serious issues is essential for timely intervention.
Common signs include persistent sadness, severe mood swings, and an overwhelming sense of fatigue. Unlike the temporary “baby blues,” which usually resolve within two weeks, postpartum depression symptoms can persist for months if untreated. Real-world examples demonstrate that early recognition of these signs can lead to better outcomes. For instance, a study found that women who received early support and intervention reported a 50% reduction in symptoms within six months.
Other notable signs include withdrawing from social interactions, experiencing difficulty bonding with the baby, and expressing doubts about one’s ability to care for the child. Data from the National Institute of Mental Health highlights that recognizing these signs early can significantly improve maternal mental health outcomes. Family members and partners play a crucial role in observing these signs and encouraging mothers to seek help.
Understanding Postpartum Depression Symptoms
Postpartum depression symptoms can range from mild to severe and may evolve over time. They often encompass emotional, physical, and cognitive dimensions, making it essential to approach this condition holistically.
Emotionally, mothers may experience feelings of hopelessness, guilt, and anxiety. These emotions can be crippling, affecting daily functioning and the ability to enjoy life. Physically, symptoms can manifest as changes in appetite, sleep disturbances, and chronic fatigue. For example, a mother might struggle with insomnia despite feeling exhausted, exacerbating her mental health challenges.
Cognitively, postpartum depression can affect concentration and decision-making. Mothers may find it difficult to focus on simple tasks or become easily overwhelmed by small decisions. It is vital to acknowledge these symptoms without judgment and seek professional postpartum support to address them effectively. Data suggests that comprehensive treatment plans, including therapy and medication, can lead to significant improvements.
Coping with Postpartum Depression
Coping with postpartum depression requires a multifaceted approach, combining self-care, professional help, and support systems. Identifying effective strategies can empower mothers to regain control over their mental health.
Self-care practices, such as regular exercise, mindfulness, and maintaining a healthy diet, can significantly impact recovery. Best practices for healing after a C-section, for example, emphasize the importance of gentle physical activity and adequate rest to support both physical and mental recovery. Engaging in activities that promote relaxation and joy can also serve as powerful antidotes to depressive symptoms.
Professional help, including therapy and medication, should be considered when symptoms persist. Cognitive-behavioral therapy (CBT) has proven effective in treating postpartum depression, helping mothers reframe negative thought patterns and develop coping strategies. Additionally, building a strong support network of friends, family, and postpartum groups can provide emotional and practical assistance, reducing feelings of isolation.
Postpartum Support and Maternal Mental Health
The role of postpartum support in enhancing maternal mental health cannot be overstated. Creating an environment where mothers feel safe to express their emotions and seek help is essential for recovery.
Community and online support groups offer platforms for mothers to share their experiences and receive empathy and guidance from others who understand their journey. These networks can be invaluable in providing reassurance and practical advice. A study on maternal support groups found that participants experienced a 40% improvement in mental health outcomes compared to those without such support.
Healthcare providers also play a critical role in offering postpartum support. Regular check-ins with a healthcare provider can help monitor a mother’s mental health and adjust treatment plans as needed. Encouraging open communication about mental health challenges during postpartum check-ups can normalize these discussions and reduce stigma.
For a more comprehensive understanding of postpartum depression and its impact, consider watching expert-led video discussions that delve deeper into personal experiences and evidence-based recovery strategies. These resources can offer visual and emotional insights that complement the information provided here.

Frequently Asked Questions
What are the main differences between baby blues and postpartum depression?
While both conditions can include mood swings and sadness, baby blues typically resolve within two weeks, whereas postpartum depression lasts longer and involves more severe emotional, physical, and cognitive symptoms. Women experiencing postpartum depression might find it difficult to function in daily life, unlike those with baby blues.
How can partners support mothers dealing with postpartum depression?
Partners can support mothers by encouraging open communication, helping with childcare and household tasks, and being patient and understanding. Accompanying them to medical appointments and participating in therapy sessions can also show solidarity and support.
Is medication always necessary for treating postpartum depression?
Medication is not always necessary; treatment plans should be personalized. Mild cases may improve with therapy, lifestyle changes, and support groups. However, medication can be beneficial for more severe cases and should be considered in consultation with a healthcare professional.
What role do healthcare providers play in postpartum mental health?
Healthcare providers play a crucial role by monitoring mental health, offering treatment options like therapy or medication, and providing referrals to support groups. Regular postpartum check-ups are opportunities to assess mental well-being and adjust care plans as needed.
Can postpartum depression affect future pregnancies?
Yes, a history of postpartum depression can increase the risk in future pregnancies. However, proactive measures, such as therapy and a strong support system, can help manage and mitigate these risks, ensuring better outcomes for subsequent pregnancies.
Conclusion
In conclusion, understanding postpartum depression is crucial in supporting mothers during one of the most transformative periods of their lives. By recognizing the signs, comprehending the symptoms, and implementing effective coping strategies, mothers can navigate this challenging time with greater resilience and support.
Next steps involve fostering open conversations about maternal mental health, encouraging early intervention, and broadening access to postpartum support networks. Healthcare providers, families, and communities must collaborate to create environments where mothers feel empowered to seek help without judgment.
If you or someone you know is struggling with postpartum depression, reach out to a healthcare provider or mental health professional today. Taking the first step can lead to a path of healing and recovery.
Further Reading
- The Impact of Postpartum Anxiety: Understanding and Addressing the Challenges
- Healing from a C-Section: Best Practices for Physical and Mental Recovery
- Building a Support System: How Friends and Family Can Help During the Postpartum Period




